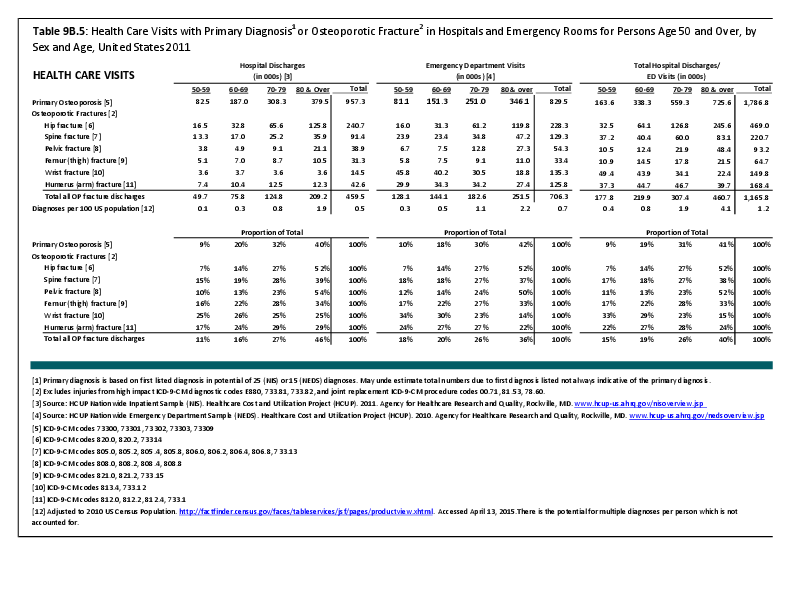
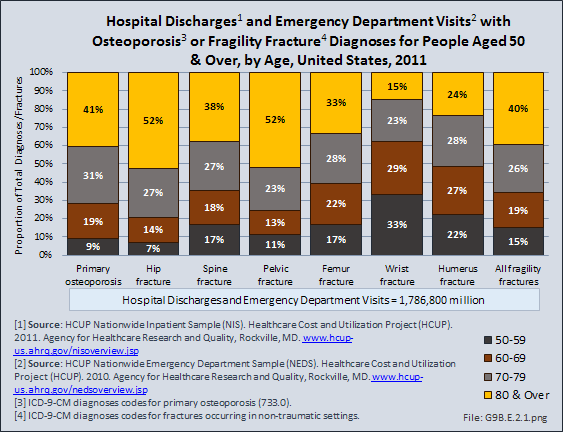
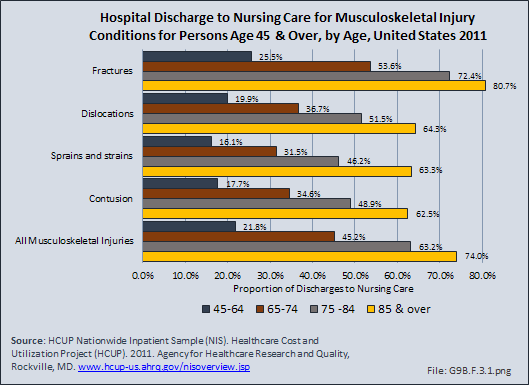
Fractures are associated with significant increases in health services utilization compared to prefracture levels. Relative to the prior 6-month period, rates of acute hospitalization are between 19.5 (distal radius/ulna) and 72.4 (hip) percentage points higher in the 6 months after fractures. Average acute inpatient days are 1.9 (distal radius/ulna) to 8.7 (hip) higher in the postfracture period. Fractures are associated with large increases in all forms of postacute care, including postacute hospitalizations (13.1% to 71.5%), postacute inpatient days (6.1% to 31.4%), home health care hours (3.4% to 8.4%), and hours of physical (5.2% to 23.6%) and occupational (4.3% to 14.0%) therapy. Among patients who were initially community dwelling at the time of the initial fracture, 0.9% to 1.1% were living in a nursing home 6 months after the fracture. These rates rose by 2.4% to 4.0% one year after the fracture.1
INSTITUTIONALIZATION
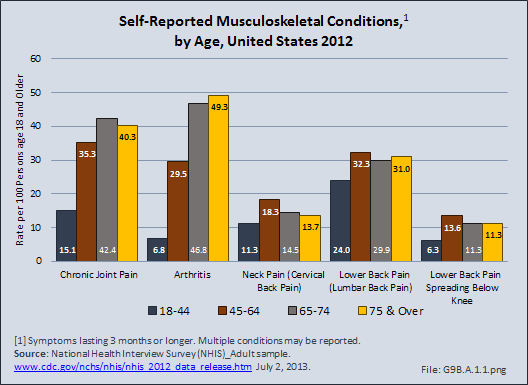
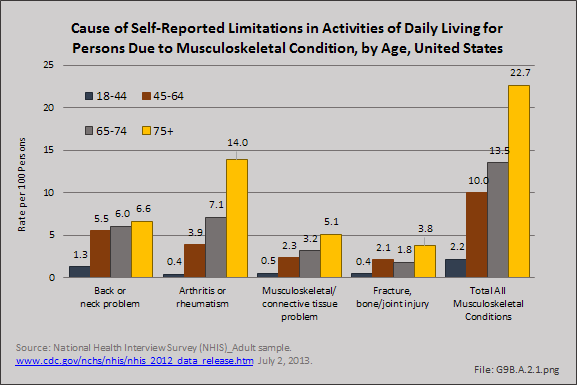
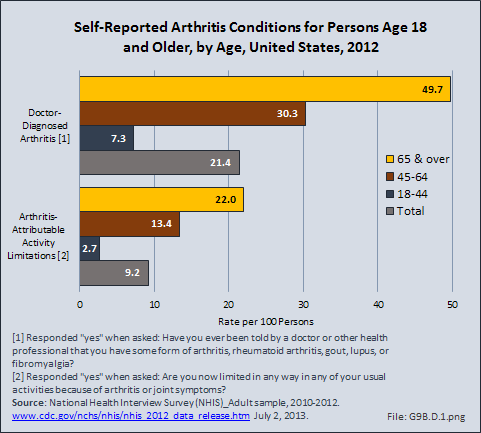
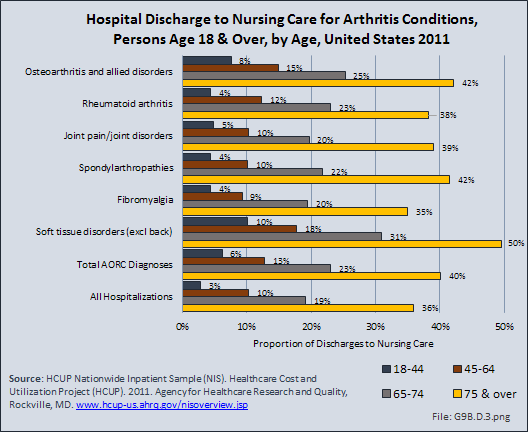
Since 1980, there has been a nearly 15% decrease in the prevalence of chronic disability and institutionalization among people aged 65 years and older. A drop in disability translates directly into cost savings since it is seven times more expensive to care for a disabled senior versus a healthy one. Major activity limitations are a common cause of nursing home admissions. While the most common cause of limitations is arthritis, affecting nearly 50% of people older than 65 years and an estimated 60 million by 2020.2 Hip fractures are a second source of immobility, and are projected to reach 289,000 in the year 2030, nearly all fall-related.3
FRACTURES AND MORTALITY
Vertebral and hip osteoporotic fractures result in a 20% increase in mortality, usually observed in the 12 months after the fracture. Men, who are generally older at the time of the hip fracture, have a 30% mortality rate after the fracture. Moreover, comorbidities such as cardiovascular disease contribute to a higher mortality rate.
A population-based study in Olmsted County, MN, found that within the first seven days after hip fracture repair, 116 (10.4%) of participants experienced myocardial infarction and 41 (3.7%) subclinical myocardial ischemia. Overall, the 1-year mortality was 22%, with no difference between those with subclinical myocardial ischemia and those with no myocardial ischemia. One-year mortality for those with a myocardial infraction was significantly higher (35.8%) than for the other two groups.4 The relative mortality after vertebral fracture varies from 1.2 to 1.9 in different reports,5,6 but the excess deaths occur late, rather than early, after vertebral fractures.5
- 1. Kilgore ML, Morrisey MA, Becker DJ, et al.: Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999–2005. J Bone Miner Res 2009;24(12):2050-2055.
- 2. National Academy on An Aging Society: Arthritis: A leading cause of disability in the United States. Chronic and Disabling Conditions. 2000;5. http://www.agingsociety.org/agingsociety/publications/chronic/index.html Accessed June 22, 2015.
- 3. Centers for Disease Control and Prevention: Hip Fractures Among Older Adults. http://www.cdc.gov/HomeandRecreationalSafety/Falls/adulthipfx.html Accessed June 22, 2015.
- 4. Huddleston JM, Gullerud RE, Smither F, et al.: Myocardial infarction after hip fracture repair: A population-based study. J Am Geriatr Soc 2012;60(11):2020-2026.
- 5. a. b. Kado DM, Browner WS, Palermo L, et al.: Vertebral fractures and mortality in older women: A prospective study. Arch Intern Med 1999;159(11):1215-1220.
- 6. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA: Mortality after all major types of osteoporotic fracture in men and women: An observational study. Lancet 1999;353(9156):878-882.
Edition:
- 2014

 Download as CSV
Download as CSV