There are many challenges to the management of patients with arthritis that need to be addressed in the future, including, but not limited to, access to specialty care for timely and accurate diagnosis, appropriate use of non-pharmacologic modailities and pharmacotherapy, including targeted small molecule and newer biologic disease modifying anti-rheumatic drugs (DMARDs), adherence to pharmacotherapy, and addressing comorbid medical conditions in patients with various forms of arthritis.
Access to Specialty Care
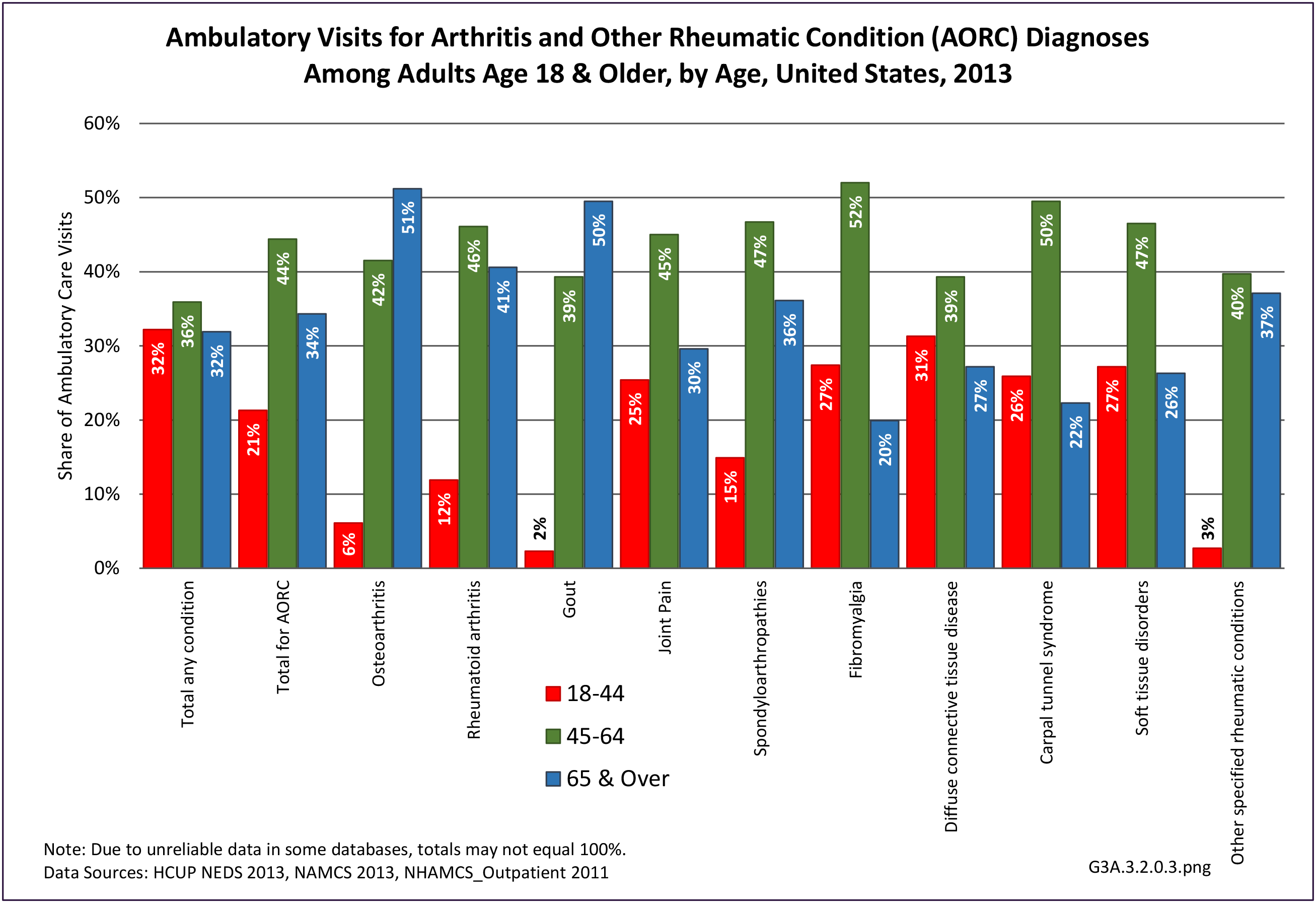
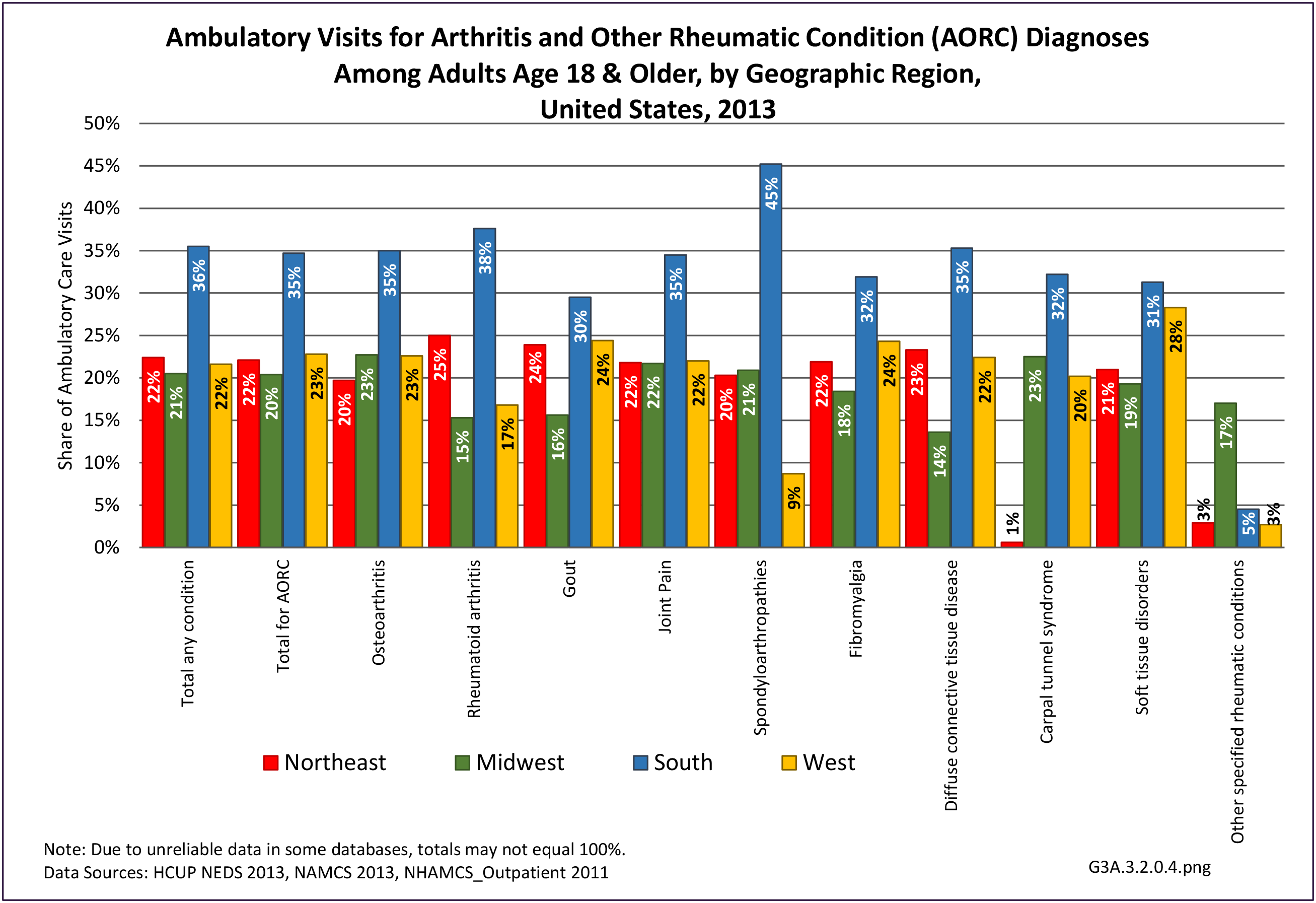
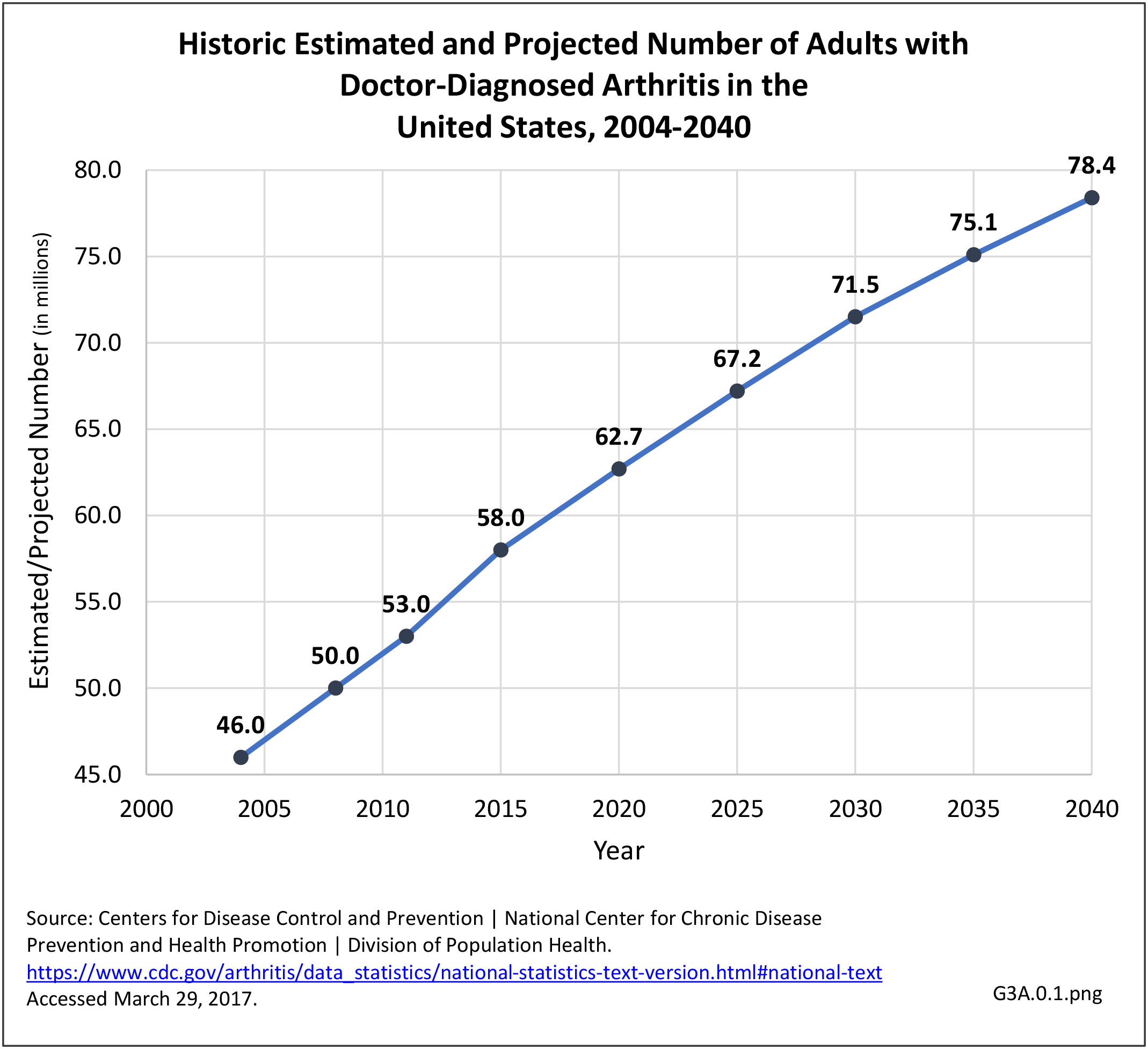
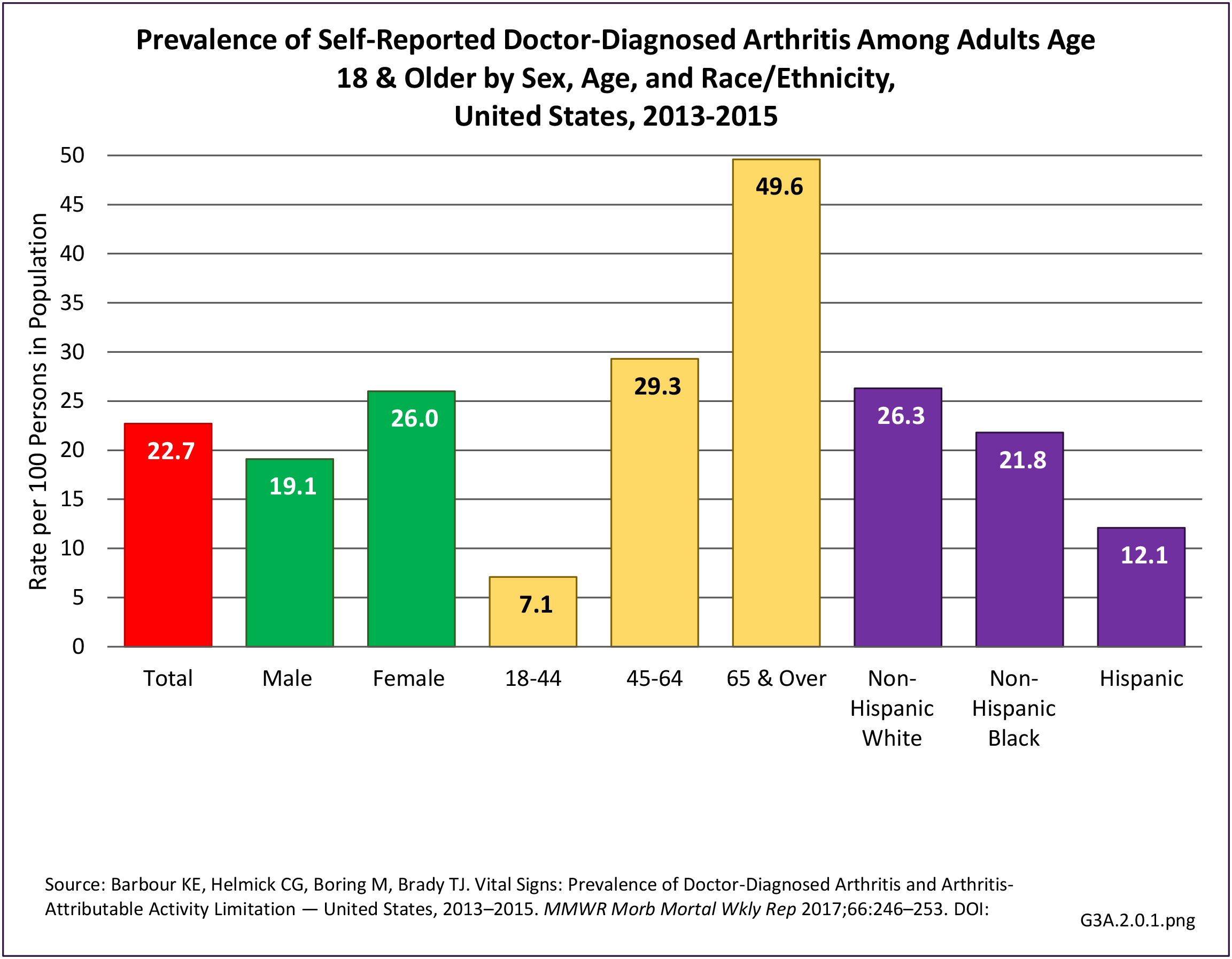
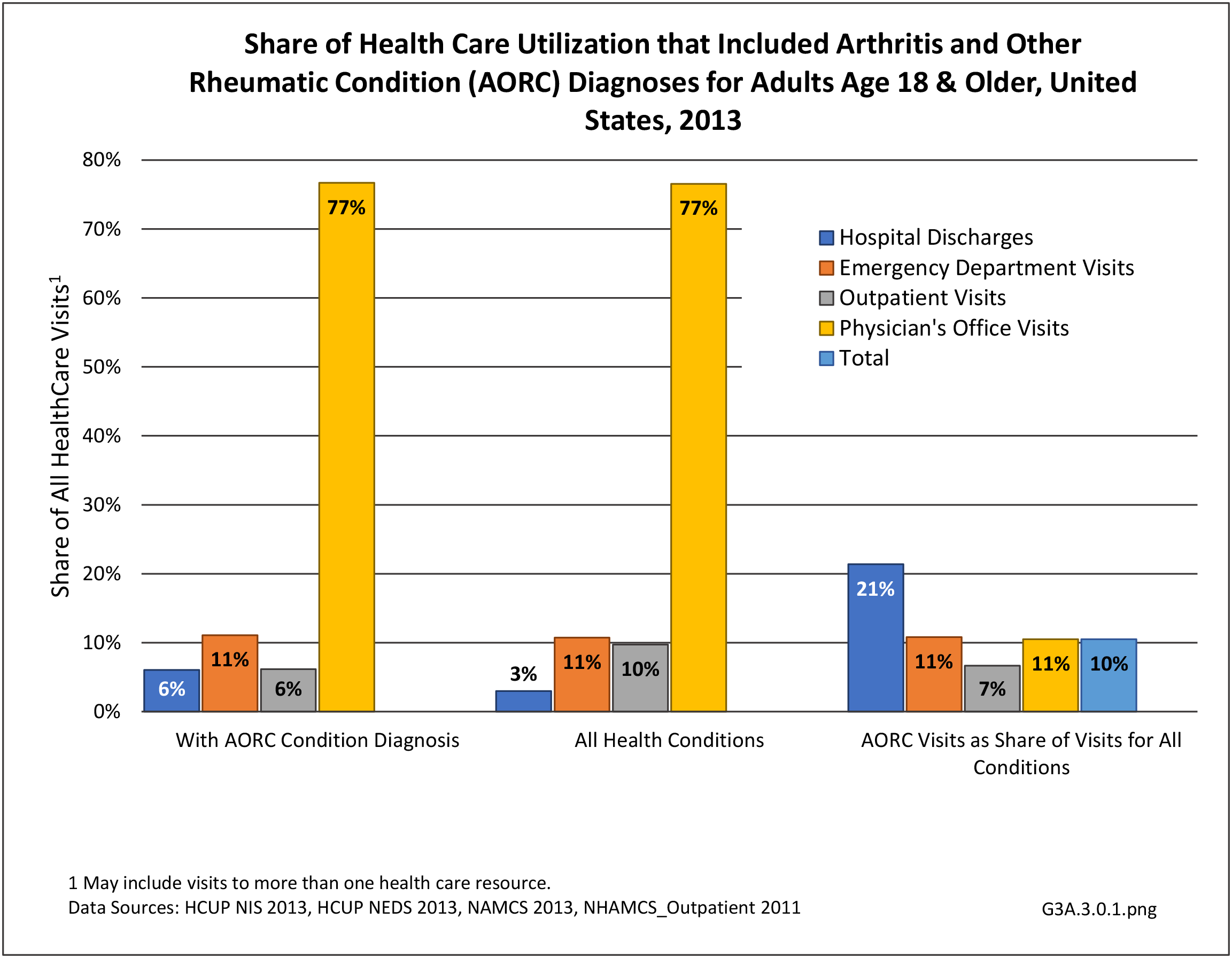
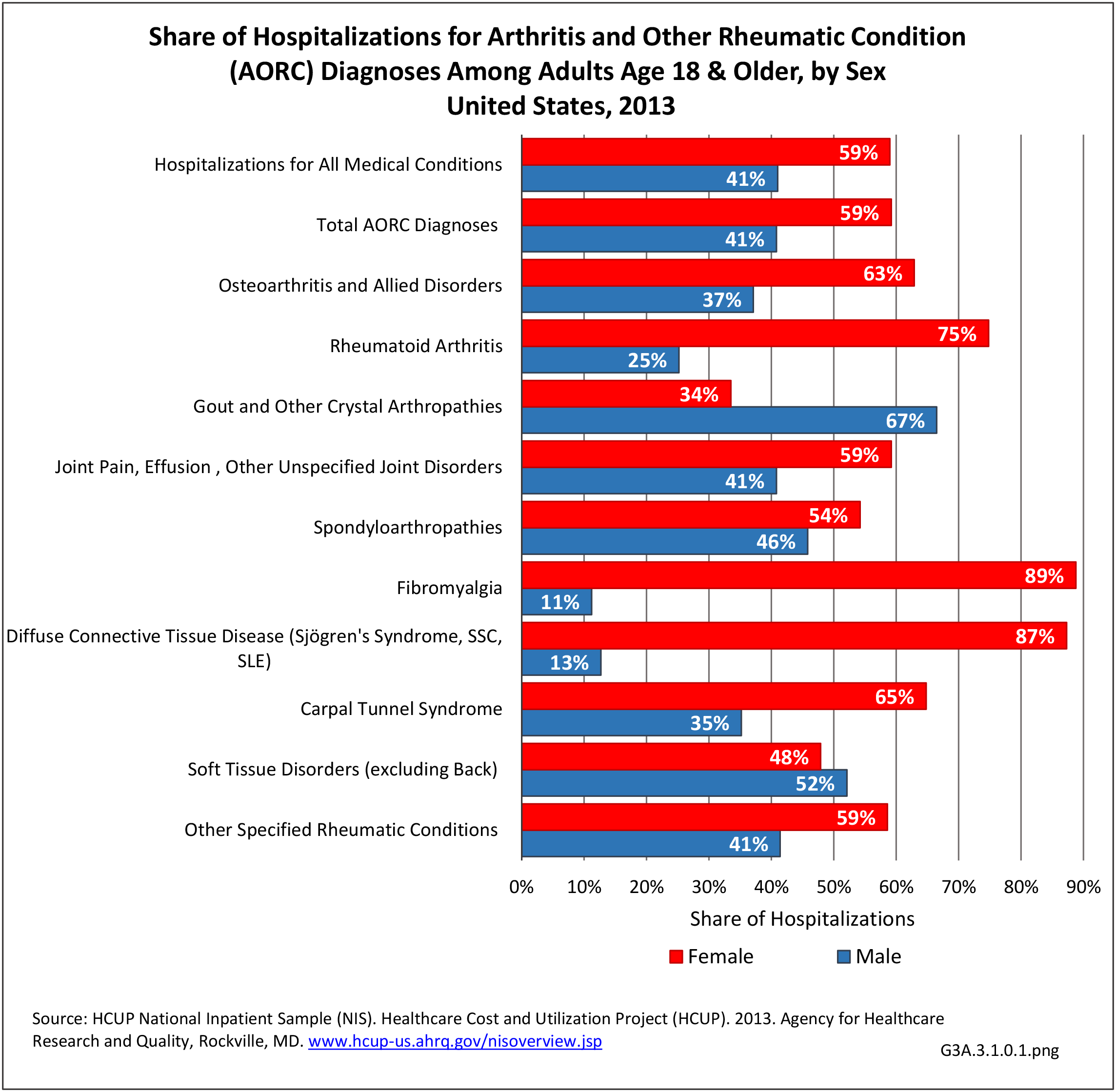
The American College of Rheumatology (ACR) conducted a workforce study in 2015 and noted that the demand for care of patients with arthritis would continue to increase with the aging of the US population.1 Major areas that were identified include the role of primary care providers in the diagnosis and management of common forms of arthritis (eg, osteoarthritis, fibromyalgia, gout) and strategies to improve options for access to rheumatologist specialty care for patients with rheumatoid arthritis, psoriatic arthritis, spondyloarthritides, and systemic autoimmune rheumatic diseases. Training of more mid-level providers (ie, nurse practitioners and physician assistants) and more health professionals (eg, nurses, physical therapists, and occupational therapists) in the care of patients with rheumatic and musculoskeletal diseases would work to address some of this demand.
In addition to issues regarding workforce, there are potential barriers to care including insurance coverage, high co-pays, and limits on number for visits for rehabilitation services such as physical therapy and occupational therapy. Adding to the cost of non-pharmacologic and pharmacologic interventions, especially newer biologic DMARDS, and pharmacy benefit reimbursement plans, are barriers due to high co-pays and prior authorization required for newer pharmacologic interventions.
Appropriate Use of Treatment Modalities
Funding of clinical trials to provide best evidence of the efficacy of treatment modalities, including non-pharmacologic interventions is needed. It is extremely important that evidence-based treatments be translated into clinical practice through the use of evidence-based recommendations published by nationally recognized professional societies. Such recommendations exist for the management of most forms of arthritis including, but not limited to, gout, osteoarthritis, rheumatoid arthritis, axial spondyloarthritis (formerly known as ankylosing spondylitis), psoriatic arthritis, and fibromyalgia. These recommendations include the use of both non-pharmacologic and pharmacologic modalities; it is felt to be important to emphasize the role of the former approaches particularly for osteoarthritis and fibromyalgia.
Adherence to Treatment Modalities
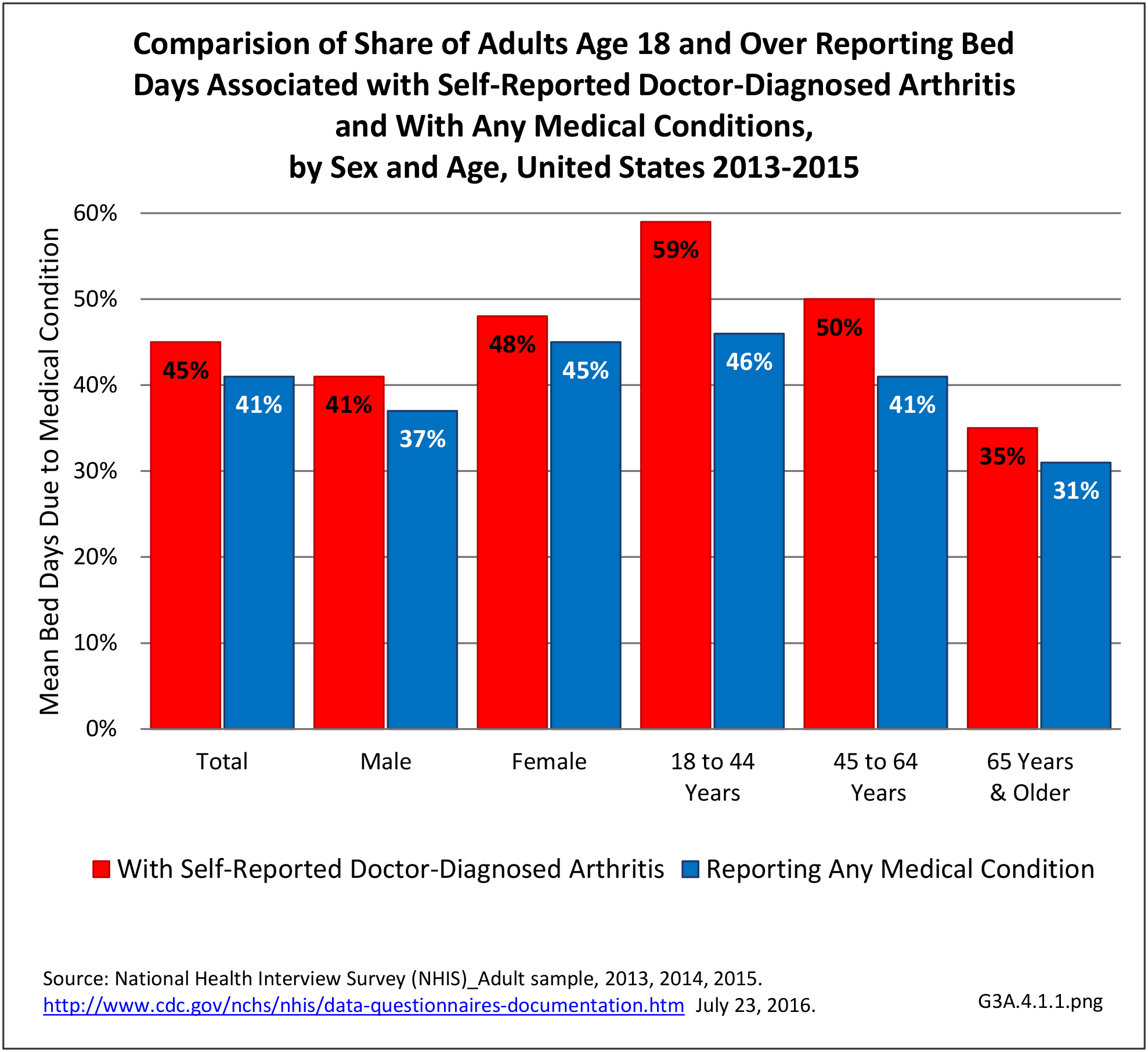
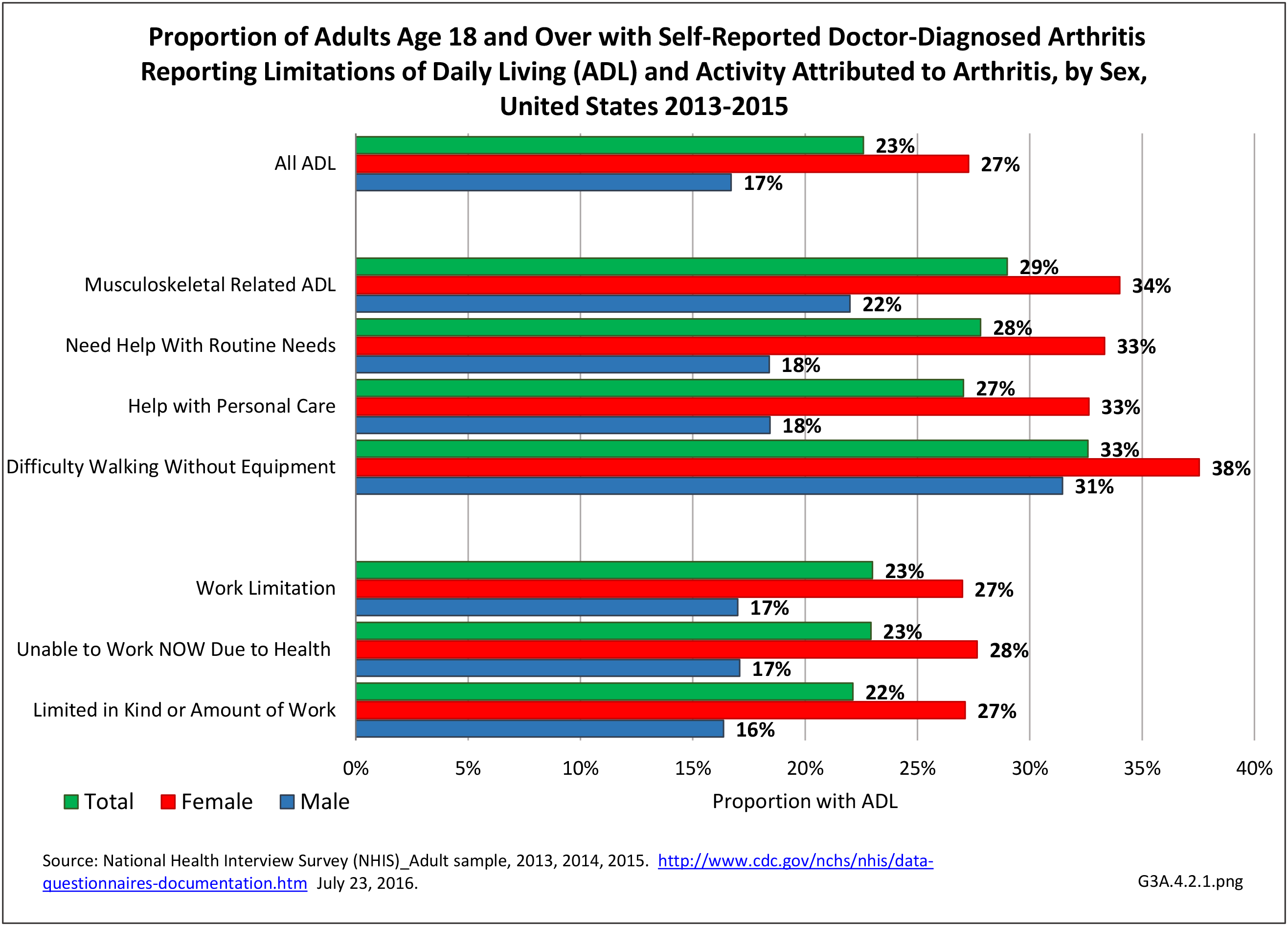
Virtually all forms of arthritis and systemic autoimmune rheumatic diseases are chronic conditions and effective treatments require patient participation, whether that is taking medications regularly (eg, urate-lowering therapy for gout) or making lifestyle changes such as adhering to dietary changes, a lifelong pattern of physical activity, or using cognitive behavioral therapy or mind-body techniques.
Management of Comorbid Medical Conditions
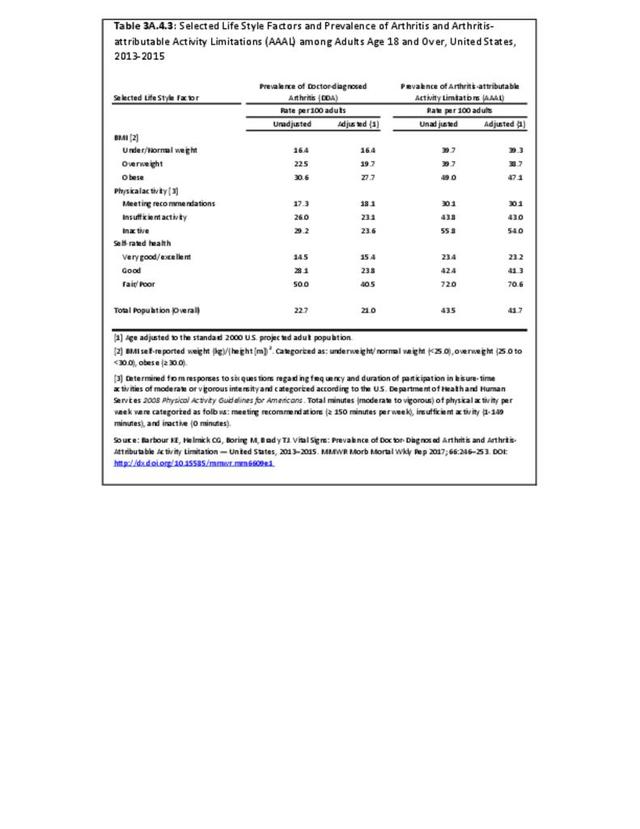
Patients with various forms of arthritis have an increased risk for cardiovascular comorbidities including coronary artery disease. While control of systemic inflammation appears to be important in ameliorating this risk, it is important for practitioners to focus on reducing other factors that contribute to increased cardiovascular disease risk including overweight and obesity, lack of physical activity, smoking, hypertension, hyperlipidemia, and poorly controlled type 2 diabetes mellitus. Depression also has been recognized as contributing to persistent pain, reduced physical function, and impaired quality of life in patients with various forms of arthritis. There is an ongoing need for care coordination between the rheumatology specialist and the primary care provider, particularly in patients who require co-management.
Meeting current and future needs will require a wealth of data currently not available or accessible. In the broad scope of musculoskeletal diseases, data currently either not available or inaccessible to BMUS analysts include treatment cost/benefits, medical workforce, geographic data at detail levels (due to small sample sizes), and outcomes.
In addition, many of the requests for additional data and analysis are beyond the scope of the current BMUS project due to staff size, staff expertise, and funding.
- 1. American College of Rheumatology. 2015 Workforce study of rheumatology specialists in the United States. Atlanta, GA. 2015. https://www.rheumatology.org/portals/0/files/ACR-Workforce-Study-2015.pdf Accessed March 26, 2018.
Edition:
- Fourth Edition